This is the fifth piece in a 12-part series on Covid. Please see the home page for previous pieces!
To summarize the series thus far, we covered Covid’s impact on the U.S. so far and how that looks relative to historical death totals, evidence-based odds on Covid infections, and responses to some of the feedback I received thus far.
Given that context, it is fair to lay out one of my main contentions, which is that lockdown and most restrictions being applied in places like the U.K., Australia, and California are simply awful policy. This is true for a number of reasons that we’ll get into over the remainder of the series.
But today’s point will be kept relatively short and focus on one of the main objections that I hear, which is around the socialized risk question. For obvious reasons, this often zooms in on hospital capacity as a key piece of that.
The argument, if I may steelman it, goes something like this:
Yes, maybe you aren’t at risk, but if we all go around only worrying about our own risk, we’ll have a huge spike in cases, overwhelm our hospitals, and we’ll see even more excess death as a result.
There is a fair basis for this thought: it is basically the tragic of the commons. If we all share low personal risk, then we can end up overusing a common resource (e.g. hospital beds) and all suffer as a result.
So let’s address a few points to counter this claim:
Personalized risk leads to different actions
The first flaw in this line is that we’ll all just go out, party like it is 2019, and create a huge spike of cases.
That’s simply not what’d happen here. Assuming accurate information provided by the government, we’d see people respond commensurate to their level of risk. This isn’t hypothetical – many states are going with the low restriction approach. But behavior largely doesn’t differ. Those who are actually at risk, or who are just paranoid, stay in. Others go out, and viral spread is kept essentially at moderate levels.
Hospital Capacity isn’t really close to being a concern
This, as I alluded to last time, is a flat out lie coming from the media. And this can be proven easily with verified data directly from the U.S. Government.
An egregious example was this recent headline from the Atlantic. “The U.S. Has Passed the Hospital Breaking Point” they cried on December 4th.
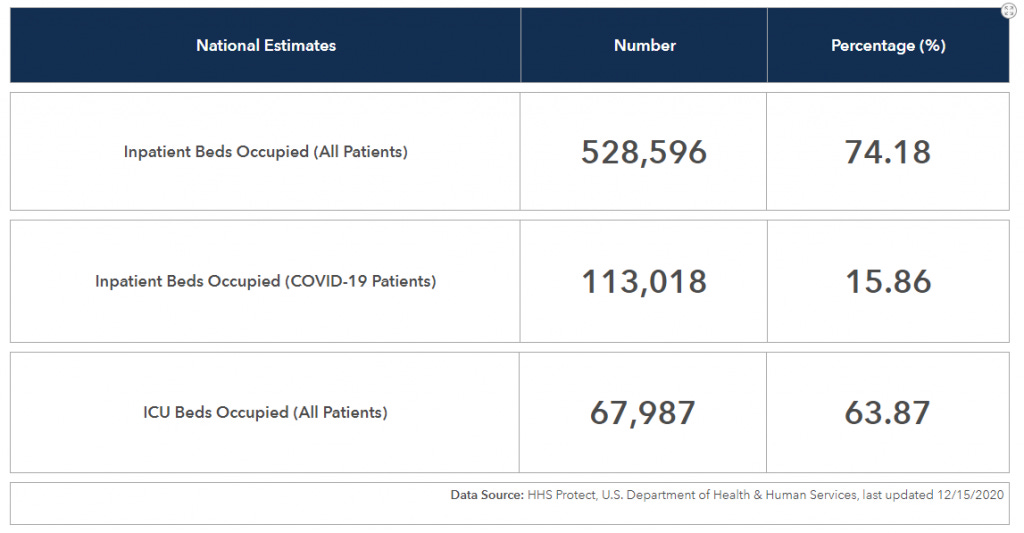
I won’t even get into what they did to try to prove this point because it honestly isn’t worth any of our time. What they could have just done is check the HHS website for data on hospital capacity (updated daily):
Now, hospitalizations have been increasing, and is higher now than it was at any point during the earlier two waves. But it’s also slowing down:
Now, obviously we’d all prefer to have less people hospitalized with Covid rather than more, barring other considerations.
But I can’t stress it enough: the claim that we’re at risk of running out of hospital space broadly (excepting some local examples), is just plain wrong.
“Spreading” the Spread is better in practice
The last point I’ll make does hinge on the contention that it is not possible for us to eliminate the virus once it becomes widespread in a population. We’ll get into this more when we look at international comparisons in a later piece, but for now accept the premise that for the U.S. trying to reign in millions of cases among 300 million people is a lot harder than Australia trying to reign in 10,000 cases among a population of 25 million.
With that said, the best course of action now is actually to do what states like Florida and Texas are doing, and not what California and New York are doing. Dare I say, Texans and Floridians are the ones “following the SCIENCE.”
Why is that? It does get back to the original mantra of “flatten the curve.” Remember that? The goal wasn’t to drive cases to zero, it was to flatten out the spread so that it was always manageable.
Here are the hospitalization rates per million for TX, FL, NY, and CA:
Obviously we see New York’s early peak. But what we see otherwise is Texas and Florida peaking in the summer, then slow rises for everyone in the fall, but with California shooting into the top spot among the four states.
We will see where California’s peak ends up. But it is quite likely it’ll be up into the 600 to 700 range given the case growth in California currently. Wait a week or two, and the two largest spikes of Covid hospitalizations will be in the states with the strictest restrictions.
That shouldn’t be surprising – we can see similar trends all around the globe. If you keep the virus in check for a bit, it will “rage” once it does get out. Let’s check out Germany, an early success:
Getting back to the broader point around socialized risks and hospital capacity, it simply falls apart as an argument on a few levels. I will reiterate: we should all be cautious and thoughtful about our actions and particularly take care around high-risk contacts.
But beyond that, there is a degree of inevitability that we all have to accept with this virus once it got loose. As we note in the last point, the “strict control” model employed by California may end up being counterproductive. At best it seems like it will head for a wash compared to more free states. And as we will get into in a future piece, the “strict control” model has huge downsides in other parts of life.